EMH Schweizerischer Ärzteverlag AG
Farnsburgerstrasse 8
CH-4132 Muttenz
+41 (0)61 467 85 44
support@swisshealthweb.ch
www.swisshealthweb.ch
Published on 01.09.2022
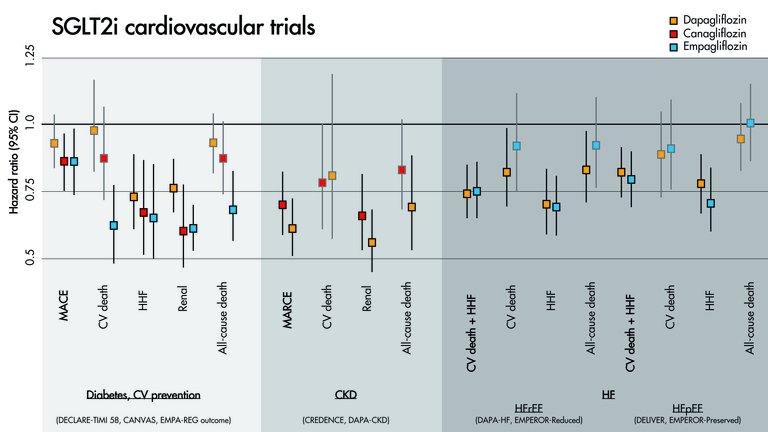
A survival kit for busy clinicians within the "SGLT2 inhibitors’ data jungle".
| Setting | Diabetes | Diabetes | Diabetes | Diabetes and CKD | CKD | HF | HF | HF | HF |
| Drug | Dapagliflozin | Canagliflozin | Empagliflozin | Canagliflozin | Dapagliflozin | Dapagliflozin | Empagliflozin | Dapagliflozin | Empagliflozin |
| Trial | DECLARE-TIMI-58 | CANVAS | EMPA-REG outcome | CREDENCE | DAPA-CKD | DAPA-HF | EMPEROR-REDUCED | DELIVER | EMPEROR-PRESERVED |
| Year | 2019 | 2017 | 2015 | 2019 | 2020 | 2019 | 2020 | 2022 | 2021 |
| Cohort | Diabetes, ASCVD or multiple risk factors, eGFR ≥60 ml/min | Diabetes, ASCVD or multiple risk factors, eGFR ≥30 ml/min | Diabetes, ASCVD, eGFR ≥30 ml/min | Diabetes, CKD (eGFR 30–90 ml/min and albuminuria) | CKD (eGFR 25–75 ml/min and albuminuria) | HF, LVEF ≤40% | HF, LVEF ≤40% | HF, LVEF >40% | HF, LVEF >40% |
| N= | 17,160 | 10,142 | 7020 | 4401 | 4304 | 4744 | 3730 | 6263 | 5988 |
| Age (y) | 64 | 63 | 63 | 63 | 62 | 66 | 67 | 72 | 72 |
| Diabetes | 100% | 100% | 100% | 100% | 67% | 42% | 50% | 45% | 49% |
| ASCVD | 41% | 72% | 100% | 50% | 37% | 56% | 51% | 57% | 35% |
| eGFR (ml/min/1.73m2) | 85 | 76 | 74 | 56 | 43 | 66 | 62 | 61 | 61 |
| HF | 10% | 14% | 10% | 15% | 11% | 100% | 100% | 100% | 100% |
| LVEF (%) | NA | NA | NA | NA | NA | 31 | 27 | 54 | 54 |
| Follow-up (y) | 4.2 | 2.4 | 3.1 | 2.6 | 2.4 | 1.5 | 1.4 | 2.3 | 2.2 |
| Primary outcome | MACE: CV death, MI, stroke | MACE: CV death, MI, stroke | MACE: CV death, MI, stroke | MARCE: CV death, renal death, ESRD, creatinine doubling | MARCE: CV death, renal death, ESRD, GFR -50% | CV death + HHF + HF urgent visit | CV death + HHF | CV death + HHF + HF urgent visit | CV death + HHF |
| HR (CI) | 0.93 (0.84–1.03) | 0.86 (0.75–0.97) | 0.86 (0.74–0.99) | 0.70 (0.59–0.82) | 0.61 (0.51–0.72) | 0.74 (0.65–0.85) | 0.75 (0.65–0.86) | 0.82 (0.73–0.92) | 0.79 (0.69–0.90) |
| All-cause mortality | 0.93 (0.82–1.04) | 0.87 (0.74–1.01) | 0.68 (0.57–0.82) | 0.83 (0.68–1.02) | 0.69 (0.53–0.88) | 0.83 (0.71–0.97) | 0.92 (0.77–1.10) | 0.94 (0.83–1.07) | 1.00 (0.87–1.15) |
| CV mortality + HHF | 0.83 (0.73–0.95) | 0.78 (0.67–0.91) | 0.66 (0.55–0.79) | 0.69 (0.57–0.83) | 0.71 (0.55–0.92) | 0.75 (0.65–0.85) | 0.75 (0.65–0.86) | 0.77 (0.67–0.89) | 0.79 (0.69–0.90) |
| CV mortality | 0.98 (0.82–1.17) | 0.87 (0.72–1.06) | 0.62 (0.49–0.77) | 0.78 (0.61–1.00) | 0.81 (0.58–1.12) | 0.82 (0.69–0.98) | 0.92 (0.75–1.12) | 0.88 (0.74-1.05) | 0.91 (0.76–1.09) |
| HHF | 0.73 (0.61–0.88) | 0.67 (0.52–0.87) | 0.65 (0.50–0.85) | 0.61 (0.47–0.80) | x | 0.70 (0.59–0.83) | 0.69 (0.59–0.81) | 0.77 (0.67-0.89) | 0.71 (0.60–0.83) |
| MACE | 0.93 (0.84–1.03) | 0.86 (0.75–0.97) | 0.86 (0.74–0.99) | 0.80 (0.67–0.95) | x | x | x | x | x |
| Renal outcomes | 0.76 (0.67–0.87) | 0.60 (0.47–0.77) | 0.61 (0.53–0.70) | 0.66 (0.53–0.81) | 0.56 (0.45–0.68) | 0.71 (0.44–1.16) | 0.50 (0.32–0.77) | x | 0.95 (0.73–1.24) |
| Reference | [3] | [4] | [5] | [6] | [7] | [8] | [9] | [10] | [11] |
Published under the copyright license.
"Attribution - Non-Commercial - NoDerivatives 4.0"
No commercial reuse without permission.
See: emh.ch/en/emh/rights-and-licences/